A case report of a person recently diagnosed with fibromyalgia
Jennifer is a 37-yr-old elementary school teacher recently diagnosed with fibromyalgia (FM).
Jennifer met with Terry Occupational Terapist in an outpatient department where Terry began the assessment with an interview using the Occupational Profile (American Occupational Therapy Association, 2017) and then completed the Canadian Occupational Performance Measure (COPM; Law et al., 2005), which focuses on client-identified problems and collaborative goal setting between therapist and client. Jennifer is a single woman who lives alone and teaches sixth grade of the scool. Jennifer reduced her work schedule to half time 3 mo ago because pain and fatigue prohibited her from being able to work in the morning. She told Terry that she is having pain in her lower legs, shoulders, and elbows. She described being independent with activities of daily living and most instrumental activities of daily living, but she admitted to having difficulty with household tasks and social activities. She said that she has not been able to resume a full-time work schedule.
Before the onset of FM, Jennifer belonged to a recreational walk–jog group, swam a couple of times a month, and went on short hikes with friends. Since the onset of her pain from FM, Jennifer described feeling “isolated.” She told Terry that she has difficulty sleeping, is gaining weight, and continues to struggle with pain. She said that she is afraid of what will happen when she runs out of narcotic pain medicine.
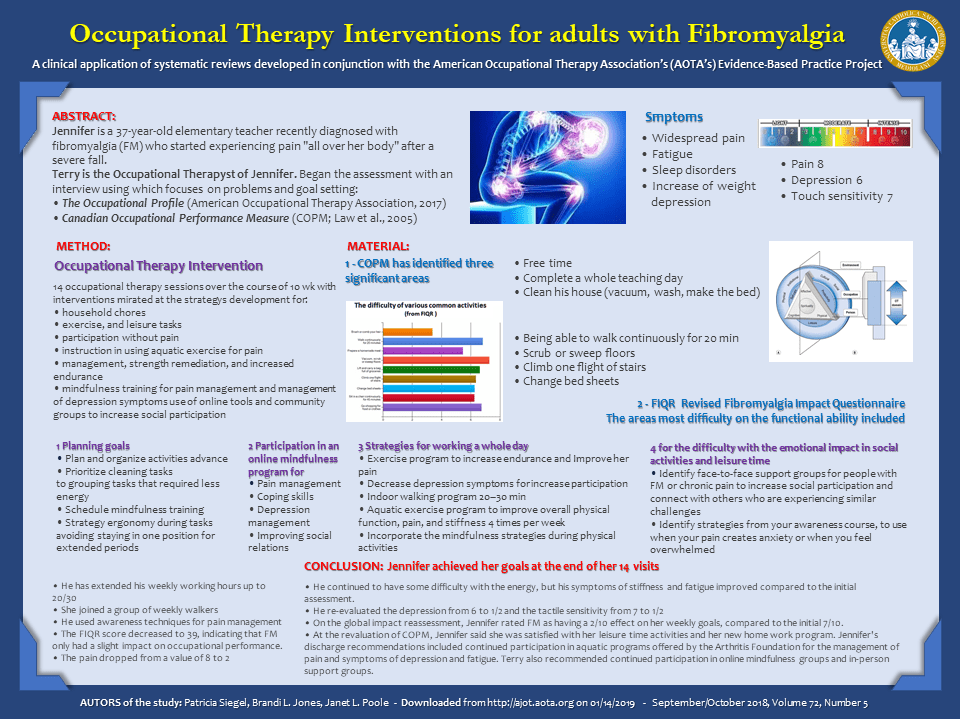
On the COPM, Jennifer identified three performance areas as being meaningful to her: leisure (being able to participate in leisure activities with friends); being able to complete a full day of teaching; and being able to clean her entire house, including vacuuming, mopping floors, and making her bed.
The areas that Jennifer indicated as presenting the most difficulty on the functional ability portion of the FIQR included being able to walk continuously for 20 min, vacuum, scrub or sweep floors, climb one flight of stairs, and change bed sheets.
Pain was an 8 on a 0–10 scale. She also indicated that she was having difficulty with anxiety, that her energy level had decreased, that she was experiencing severe stiffness, and that she was waking from sleep still feeling tired. Depression level and tenderness to touch were rated at a 6 and 7, respectively, on a 0–10 scale.
Occupational Therapy Intervention
Jennifer received 14 occupational therapy sessions over the course of 10 wk. These sessions included the following interventions: instruction in routine development for household chores, exercise, and leisure tasks with a focus on participation without pain; instruction in using aquatic exercise for pain management, strength remediation, and increased endurance; mindfulness training for pain management and management of depression symptoms; and use of online tools and community groups to increase social participation. Terry planned these interventions, in conjunction with Jennifer.
INTERVENTION 1
1.Plan tasks in advance
2.Prioritize cleaning tasks
3.would rate the task on a scale of 1–10 to indicate how much time and energy she had spent with the task as well as her fatigue after the task
4.Plan and organize activities. Terry instructed Jennifer to group tasks that required less energy (e.g., grading student papers, paying bills) with those that were more taxing, such as vacuuming. She also suggested that Jennifer schedule and plan rest periods during which she could do mindfulness training.
5.Use good posture and body mechanics during tasks. Terry instructed Jennifer to avoid staying in one position for extended periods and to change her position often. She also advised her to use good body mechanics during vacuuming, including using larger joints to move the vacuum and lifting with her legs when picking it up.
INTERVENTION 2
Jennifer identified pain management and fatigue as considerable barriers to her occupational participation. Terry recommended participation in an online mindfulness program for pain management, coping skills, depression management, and improving social relations.
INTERVENTION 3
To address Jennifer’s goal of working a full day, Terry developed an exercise program to increase Jennifer’s endurance, improve her pain, and decrease depression symptoms that affected participation. Terry recommended an indoor walking program (Mannerkorpi et al., 2010) and implemented an aquatic exercise program to improve overall physical function, pain, and stiffness (Bidonde et al., 2014). Jennifer was instructed in light resistance exercises in the aquatic environment and completed 20–30 min of indoor walking at least 4 times per week. and instructed Jennifer to incorporate the mindfulness strategies from her online course during physical activities.
INTERVENTION 4
During the assessment process, Jennifer indicated difficulty with the emotional impact of FM and that this condition was preventing her from participating in social and leisure activities as much as she would like. Terry worked with Jennifer to identify face-to-face support groups for people with FM or chronic pain to increase her social participation and toconnect her with others who are experiencing similar challenges. In addition, Terry worked with Jennifer to identify strategies from her mindfulness course to use when her pain creates anxiety or when she is feeling overwhelmed.
CONCLUSION
With evidence-based and client-centered occupational therapy interventions, Jennifer met her goals at the end of her 14 visits. Jennifer increased her weekly work hours from 20 to 30, joined a weekly walking group, and was using mindfulness techniques for pain management. Jennifer’s FIQR score on discharge was 39, indicating that FM had a mild impact on occupational performance. On the symptom portion of the FIQR, Jennifer reported having pain corresponding to 2 on a 0–10 scale. She continued to have some difficulty with energy, but her symptoms of stiffness and fatigue improved from the initial evaluation. She rated feeling depressed and very tender, between 1 and 2 on a 0–10 scale, a considerable decrease from the initial rating of 6 or 7. On the global impact portion of the FIQR, Jennifer rated FM as having a 2/10 effect on her weekly goals, down from 7/10 at evaluation. On her discharge COPM, Jennifer indicated that she was satisfied with her leisure activities and new work schedule and that she felt that the cleaning schedule helped her allocate vacuuming and other household tasks. Jennifer’s discharge recommendations included continued participation in the aquatic programs offered by the Arthritis Foundation for the management of pain and symptoms of depression and fatigue. Terry also recommended continued participation in online mindfulness groups and in-person support groups.
Lascia un commento